About Age-Related Macular Degeneration
Macular degeneration is a term which includes hundreds of conditions affecting the macula. In this section we will be discussing age-related macular degeneration (AMD) also known as age-related maculopathy. AMD is the leading cause of blindness in adults over 55 years of age in the United States. The macula is the part of the retina responsible for central vision. This detailed vision is important for reading, watching TV and driving as well as any task requiring fine vision. The macula is the part of the retina most affected by macular degeneration.
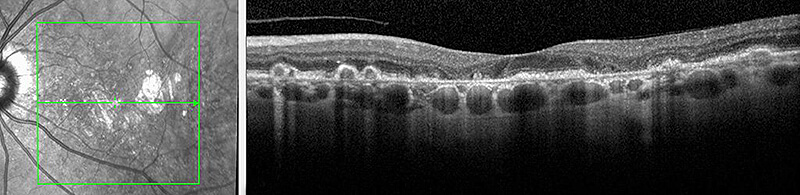
The retina is made up of several layers which line the inner wall of the eye. Each layer has a specific function and all work together to create vision. When light enters the eye it is focused by the cornea and lens onto the macula. The light is then converted into electrical signals by cells in the retina called photoreceptors. These photoreceptors send signals to the brain via the optic nerve which are then interpreted by the vision centers in the brain. In AMD, these cells or photoreceptors break down over time and eventually accumulate under the retina. These accumulations appear as yellow deposits called drusen. It is believed that drusen and associated waste products prevent adequate nutrition from reaching the retinal cells. The characteristics of these drusen and the amount of damage to the macula are used to determine the severity of AMD. Usually, as the number and size of drusen increases, the severity of AMD increases and visual symptoms worsen.
AMD is divided into two general categories, dry AMD (DAMD) and wet AMD (WAMD). A simple way to think about these two categories is that in WAMD there are abnormal blood vessels growing under or in the retina which may leak blood and fluid, while in DAMD there are no abnormally growing blood vessels. Dry AMD often results in a gradual loss of vision while wet AMD may result in a sudden and sometimes more severe loss of vision.
Dry Macular Degeneration (DAMD)
Approximately 90% of patients with AMD have the dry form. Dry macular degeneration is often divided into three stages – early, intermediate and advanced. Early stage DAMD begins with the formation of small drusen. There may not be any loss of vision at this stage. However, as more drusen develop and become larger (intermediate DAMD) the central vision may slowly become blurry, dim or faded. In advanced DAMD the build up of drusen eventually causes associated retinal cells to die. The process of cell death is called atrophy. If the disease progresses these areas of atrophy can become larger and more dense, causing further damage to the macula. Over time this can result in a significant decrease in central vision.
Wet Macular Degeneration (WAMD)
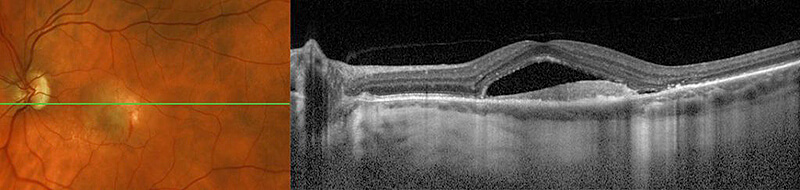
Approximately 10% of patients with AMD have the wet form. Patients with wet AMD start out with the dry form of AMD initially. In WAMD, abnormal blood vessels start growing within or underneath the retina from a layer called the choroid. The growth of these abnormal blood vessels is called choroidal neovascularization (CNV) and can lead to the leakage of fluid and blood which defines WAMD. With the pooling of fluid and blood underneath the photoreceptor layer (the layer responsible for transmitting signals to the brain) the retina is no longer able to function normally which often causes a sudden change in vision. The abnormal blood vessels and bleeding can also cause further scarring (fibrosis) of the retina. Scarring from WAMD in the macula may cause an irreversible loss of central vision.
Treatment of Wet AMD
Wet AMD occurs when abnormal blood vessels grow within or underneath the retina. They usually grow from the choroid layer which lies under the retina but they can also occur from the retina as well.
There are numerous treatments available for these abnormally growing and leaking blood vessels including: intravitreal injections, thermal laser, photodynamic therapy (PDT) or a combination of these treatments.
For additional information, please visit the ASRS page on age-related macular degeneration.
For additional information please visit the National Eye Institute page on macular degeneration or the ASRS page on macular degeneration.
